Helping people to live and survive co-use of benzodiazepines/z-drugs and opioids: the importance of asking how and why people co-use
Helping people to live and survive co-use of benzodiazepines/z-drugs and opioids: the importance of asking how and why people co-use
Gabriele Vojt, Joanna Kesten, Jennifer Scott, Hannah Family, on behalf of the Benzo Opioid study team
Dr Gabriele Vojt is an academic researcher at the University of Bristol where she works closely with a team of qualitative researchers (JS, JK, HF), with expertise in health and behavioural psychology (HF), mental health (GV, HF, JK, JS) and pharmacy (JS) in public health.
In a recent webinar, we shared findings from our research study to understand the relationships between co-using benzodiazepines (e.g., diazepam) or z-drugs (e.g., zopiclone) and opioid use (for example, heroin or methadone) and drug-related deaths. In this blog, we highlight findings around how and why people use benzodiazepines/z-drugs and opioids together.
A research study to understand co-use of benzodiazepines/z-drugs and opioids
We spoke with 48 people (living in Scotland, North or South-West England) who co-use opioids and benzodiazepines/z-drugs at the same time or in a short time frame (depending on drugs, this could be minutes to hours). We found that everyone we spoke to also used other drugs like stimulants (cocaine) and alcohol. Most people had overdosed or been unconscious after they had used drugs and had poor mental health. This included feeling anxious and depressed, but also official diagnoses like psychosis (e.g., schizophrenia) and post-traumatic stress disorder, which were often linked to painful and abusive experiences in people’s childhood and/or adulthood.
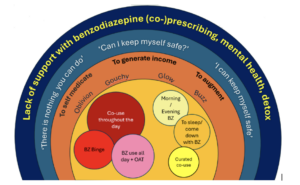
Six different ways of combining drugs
We identified six ways in which people used these drugs together: (1) ‘Co-use throughout the day’ (daily, high doses), (2) ‘Benzodiazepine binge’ (occasional, high doses over 1-3 days), (3) ‘Benzodiazepine use all day on top of opioid substitution therapy’ (daily, high doses of benzodiazepines), (4) ‘curated co-use’ (carefully chosen doses of opioids and benzodiazepines, situation specific), (5) ‘to sleep or come down with benzodiazepines’ (evening benzodiazepines, usually low dose), and (6) ‘morning/evening dose of benzodiazepines’ (low dose, morning and evening). The patterns differ in how much control people felt they had over the quantity, dosage and frequency with which they used these drugs. We checked our findings with experts with lived experience, and we learned that some people stuck to the same pattern, but for others, their patterns could change in response to things that happened during a person’s day or when things were changed with their prescribed medicine – e.g. change to their opioid substitution treatment.
Why do people use different drugs together at the same time?
Often the reasons were functional: people needed drugs to get through the day, make it out of the house, attend appointments, manage sleep problems or tried to self-medicate poor physical health (chronic pain) or poor mental health (anxiety, depression). At the same time, people also told us about the experiences and feelings they were seeking; these ranged from wanting to forget (‘oblivion’), feeling relaxed (‘gouch out’) to wanting to feel good and happy (‘buzz’ or ‘glow’). Most of the time, people said they just wanted to feel ‘normal’ for a little bit.
What do people do to keep themselves safer when co-using drugs?
We asked people what they thought about their risk of overdosing and what they did to keep safe. People often wondered ‘can I keep myself safe?’ when using illegally obtained drugs. People were worried about their risk of overdosing. Some people tried hard to stay safe, and they adapted harm reduction advice and strategies, often learned and developed from their own trial and error. However, there were some people who spoke of hopeless- and helplessness and they did not believe that anyone or anything could help them to stay safe. This belief ‘there is nothing you can do’ was linked to a perception that treatment and support offers did not meet their needs or were not accessible for them.
© 2025 University of Bristol
The need for mental health support to help people live and manage their drug use
People who use benzodiazepines/z-drugs and opioids (often with other drugs) told us about three major things that they feel are needed: mental health support (psychosocial interventions), access to benzodiazepine prescriptions (with or without optimised opioid substitution therapy) and help to detox in the community. We then spoke to staff to get their views on what was missing for service providers who wanted to help people who co-use drugs. Staff were reluctant to prescribe benzodiazepines and opioids because they felt that there was not enough evidence on how safe or effective it was. There was also a need for more guidance on how staff could best support people who are dependent on both drugs (especially in England). Staff were also worried that without access to appropriate mental health support, people would struggle to cope with benzodiazepine detox or abstinence.
Recommendations for practice and future research
From our research, we suggest six recommendations. We developed these recommendations together with academics, practitioners, people with lived and living experience and policy makers.
- A flexible, tailored approach to normalise prescribing to help people live/function.
- Specialist mental health support tailored to individuals who use are co-using benzodiazepines/z-drugs and opioids.
- Holistic psychosocial interventions aimed at improving people’s everyday health, resilience and wellbeing.
- Clear and accessible harm reduction information including effects of different benzodiazepines, drug interactions and drug administration routes.
- Upskill staff to better understand the effects and interactions between benzodiazepines/z-drugs and other drugs.
Our next steps are to do more work with mental health practitioners, to develop and test a way of improving the support for people who use benzodiazepines/z-drugs and opioids.
Further reading
Family HE, Vojt G, Poulter H, Bailey CP, Abdala Sheikh AP, Cavallo D, Karimi S, Booth N, Da Silva P, Aitken L, Stewart S, Hickman M, Henderson G, Scott J, Kesten JM. A qualitative study of benzodiazepine/z-drug and opioid co-use patterns and overdose risk. Harm Reduct J. 2025 Feb 27;22(1):24. https://pubmed.ncbi.nlm.nih.gov/40016748/
Vojt G, Family HE, Poulter H, Bailey CP, Cavallo D, Abdala Sheikh AP, Karimi S, Booth N, Da Silva P, Aitken L, Stewart S, Hickman M, Henderson G, Scott J, Kesten JM. Motivations underlying co-use of benzodiazepines and opioids in the UK: a qualitative study. Harm Reduct J. 2025 Sep 29;22(1):152.https://pubmed.ncbi.nlm.nih.gov/41024026/
Can I keep myself safe? Experiences of Benzodiazepine/Z-drug and opioid co-use. Research findings and recommendations for drug treatment and mental health service provision. [short summary of our findings]. Benzo-Opioid-Booklet-FINAL-PDF.pdf
More information and background on our project website: